COVID-19 On Hospitals : With the onset of the COVID-19 pandemic, hospitals around the world faced unprecedented challenges that tested their capacity, resources, and resilience. The impact of the virus on healthcare systems was profound, highlighting both strengths and weaknesses in the way hospitals operate. As we reflect on the lessons learned from this experience, it is vital to examine how we can better prepare for future health crises.
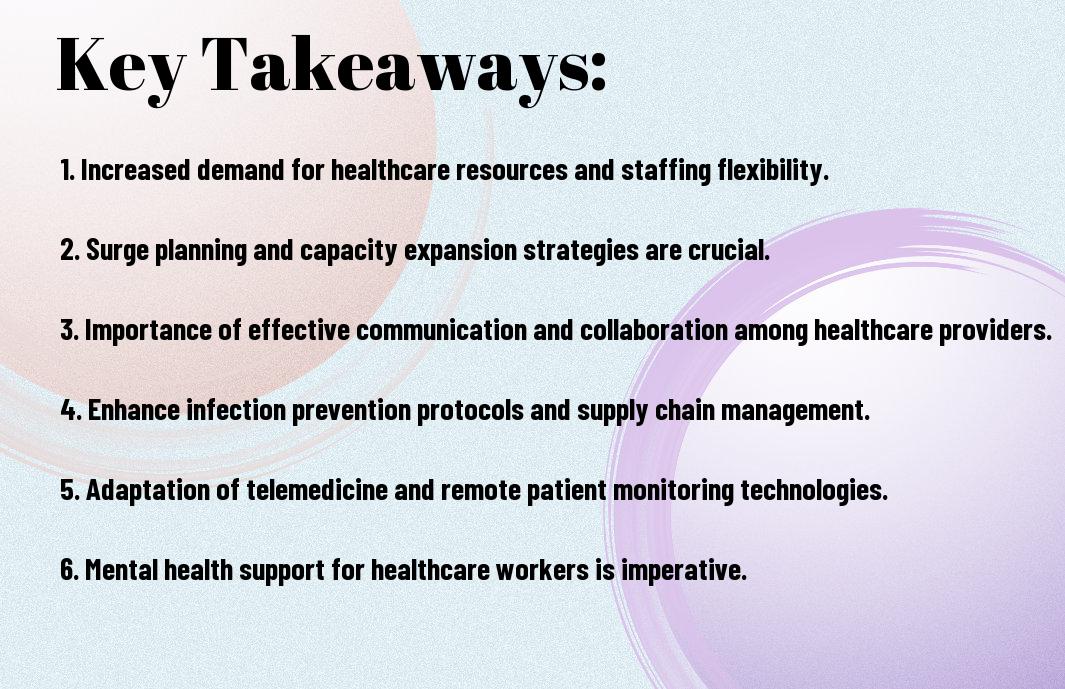
Key Takeaways:
- Importance of Preparedness: The COVID-19 pandemic highlighted the critical importance of having robust preparedness plans in place at hospitals to effectively respond to healthcare crises.
- Need for Flexibility and Scalability: Hospitals must be adaptable and scalable to quickly adjust to surges in patient numbers, supply shortages, and changing guidelines during a crisis like the pandemic.
- Emphasis on Communication and Collaboration: Effective communication and collaboration between hospitals, healthcare providers, government agencies, and the community are imperative for a coordinated response and optimal patient care outcomes during a healthcare emergency.
The Immediate Impact on Hospitals
While the world was caught off guard by the rapid spread of the COVID-19 pandemic, hospitals found themselves at the frontlines of the battle. The immediate impact on hospitals was overwhelming, exposing weaknesses in the healthcare system and highlighting the need for preparedness for future crises.
Challenges in Managing Patient Influx
Impact Hospitals faced a surge of patients seeking care for COVID-19 symptoms, putting a strain on resources, staff, and infrastructure. Emergency departments were inundated, hospital beds reached capacity, and healthcare workers were stretched thin, trying to manage the influx while maintaining quality care.
Impact The challenges in managing patient influx not only tested the resilience of hospitals but also exposed gaps in coordination between healthcare facilities. The lack of a unified approach to patient triage and transfer exacerbated the strain on already overwhelmed hospitals, leading to delays in care and impacting patient outcomes.
Effects on Healthcare Workers and Hospital Resources
With the rapid increase in patients requiring intensive care, healthcare workers faced unprecedented levels of stress, fatigue, and burnout. PPE shortages further added to the challenges, putting frontline workers at risk and forcing hospitals to ration necessary resources to protect their staff.
It became clear that the well-being of healthcare workers is paramount to sustaining the healthcare system during a crisis. The effects of the pandemic on the mental and physical health of frontline workers highlighted the need for better support systems and resources to ensure their safety and resilience.
Disruptions to Routine Care and Elective Procedures
Healthcare facilities had to make difficult decisions to cancel or postpone elective procedures and routine care to prioritize resources for COVID-19 patients. This led to delays in necessary medical care for non-COVID-19 patients, raising concerns about the long-term impact on public health.
This disruption highlighted the delicate balance that hospitals must maintain between managing COVID-19 cases and providing necessary healthcare services to the broader population. The lessons learned from these disruptions will inform future preparedness strategies to ensure continuity of care in times of crisis.

Infection Control and Hospital Response
All hospitals faced unprecedented challenges during the COVID-19 pandemic, requiring them to implement strict infection control measures to protect both patients and healthcare workers. The adoption of new hygiene practices became imperative to prevent the spread of the virus within healthcare facilities.
Implementation of New Hygiene Practices
Practices such as frequent handwashing, the use of personal protective equipment (PPE), and enhanced cleaning protocols were introduced and strictly enforced. Hospitals initiated comprehensive training programs to ensure that all staff members were well-versed in the latest infection control guidelines and practices.
These measures not only helped in containing the spread of COVID-19 within hospitals but also significantly reduced the risk of healthcare-associated infections. The heightened awareness of infection control practices cultivated a culture of safety and vigilance among hospital staff, fostering a more resilient healthcare system.
Development of COVID-19 Specific Protocols
With the evolving nature of the pandemic, hospitals developed COVID-19 specific protocols to streamline their response efforts. These protocols outlined procedures for patient screening, isolation, and treatment, ensuring a standardized approach to managing COVID-19 cases.
Implementation of these protocols facilitated efficient patient flow and resource allocation, optimizing hospital operations amidst the crisis. Hospitals collaborated with public health authorities and infectious disease specialists to continuously update and refine these protocols based on emerging evidence and best practices.
Role of Isolation Units and Redesigning Hospital Spaces
Response to the surge in COVID-19 cases necessitated the establishment of dedicated isolation units within hospitals to care for infected patients while preventing cross-contamination. Hospital spaces were redesigned to accommodate the increased demand for isolation rooms and ensure proper ventilation to reduce the risk of viral transmission.
Specific attention was given to the design and layout of these units to enhance infection control measures, with barriers, negative pressure rooms, and strict access controls put in place to contain the virus effectively. These measures were crucial in protecting vulnerable populations and preventing outbreaks within healthcare facilities.
Financial Implications for Healthcare Systems
Economic Burden on Hospitals
Unlike any other crisis in recent history, the COVID-19 pandemic has placed an immense economic burden on hospitals worldwide. The sudden surge in patients requiring intensive care and specialized treatment overwhelmed healthcare systems, leading to increased costs for medical supplies, equipment, and staffing.
Hospitals struggled to keep up with the rising expenses as revenues plummeted due to canceled elective procedures and the shift towards caring for COVID-19 patients. Many healthcare facilities faced financial strain, with some even at risk of closure as a result of the pandemic’s impact on their bottom line.
Impact on Healthcare Funding and Reimbursement Models
Any disruption in healthcare delivery, such as the one caused by COVID-19, has significant repercussions on funding and reimbursement models. The pandemic highlighted the limitations of fee-for-service models and exposed the vulnerabilities of healthcare systems reliant on this traditional payment structure.
Funding streams were disrupted, and healthcare providers found themselves in a precarious position as they struggled to maintain financial viability while continuing to provide vital care to their communities. The pandemic underscored the need for a more resilient and adaptable funding and reimbursement framework in the face of future crises.
For instance, hospitals and healthcare systems must explore innovative payment models, such as value-based care and capitation, to ensure financial stability and sustainability in times of uncertainty. Embracing technology and telehealth solutions can also help optimize revenue streams and improve cost-efficiency in the long run.
Technology and Innovation in the Pandemic
Adoption of Telemedicine and Remote Patient Monitoring
Not only has the COVID-19 pandemic brought a wave of challenges to the healthcare system, but it has also catalyzed the adoption of telemedicine and remote patient monitoring technologies. With the need to limit in-person interactions and reduce the risk of virus transmission, healthcare providers have rapidly implemented virtual care solutions. Patients can now consult with their healthcare providers from the comfort of their homes, reducing the burden on hospital resources and minimizing exposure to the virus.
These technologies have not only improved access to care but have also enhanced efficiency and convenience for both patients and healthcare professionals. Virtual consultations have allowed for timely assessments, continuous monitoring of patients’ health status, and real-time interventions when necessary. The pandemic has highlighted the significance of telehealth in providing healthcare services in a scalable and sustainable manner.
Information Technology and Data Management
On the front lines of the pandemic, information technology and data management have played a critical role in supporting healthcare delivery and decision-making processes. Through robust electronic health record systems and data analytics tools, hospitals have been able to track the spread of the virus, monitor patient outcomes, and optimize resource allocation. The ability to quickly access and analyze data has been instrumental in guiding response efforts and improving overall patient care.
Any delay or inefficiency in data management could have severe repercussions during a public health crisis. Therefore, investing in information technology infrastructure and optimizing data management processes is crucial for healthcare organizations to effectively respond to future challenges. The pandemic has underscored the importance of leveraging technology to collect, analyze, and interpret data in real-time to make informed decisions and improve patient outcomes.
Advancements in Medical Equipment and Supplies
Supplies of vital medical equipment and supplies faced unprecedented challenges during the peak of the pandemic. Hospitals grappled with shortages of ventilators, personal protective equipment, and other critical supplies necessary for patient care. However, the crisis has spurred innovation and collaboration in the healthcare industry, leading to the development of new medical devices, rapid production methods, and enhanced supply chain management strategies to meet the increased demand.
The pandemic has demonstrated the need for preparedness and resilience in the healthcare supply chain. Moving forward, healthcare providers must invest in advanced medical equipment and supplies, diversify sourcing options, and establish contingency plans to ensure uninterrupted access to critical resources during times of crisis. The lessons learned from the pandemic underscore the importance of innovative solutions and strategic partnerships in enhancing healthcare delivery and response capabilities.
Information: Amid the challenges posed by the COVID-19 pandemic, technological advancements and innovative solutions have reshaped healthcare delivery and preparedness efforts. From telemedicine adoption to data management enhancements and advancements in medical equipment and supplies, the industry has shown remarkable resilience and adaptability in the face of unprecedented challenges. Moving forward, leveraging technology and innovation will be key to improving healthcare outcomes, enhancing patient experiences, and strengthening healthcare systems against future threats.
Hospital Workforce Adaptations and Well-being
Despite the unprecedented challenges posed by the COVID-19 pandemic, hospitals have shown remarkable resilience in adapting their workforce strategies to meet the surge in patient numbers and the changing demands on healthcare systems. The well-being of healthcare workers has become a critical focus as hospitals navigate staffing challenges, provide mental health support systems, and prioritize training and education to ensure preparedness for future crises.
Staffing Challenges and Workforce Redevelopment
Wellbeing of healthcare workers has been a paramount concern as hospitals face shortages in staff due to illness, burnout, and increased workload. Many healthcare facilities have implemented innovative strategies such as redeploying non-clinical staff to support frontline workers, hiring temporary staff, and offering incentives to retain experienced employees. These adaptations have been necessary in maintaining high-quality patient care while safeguarding the physical and mental health of the hospital workforce.
Redevelopment of workforce skills and roles has been a key strategy in addressing staffing challenges during the COVID-19 crisis. Hospitals have focused on cross-training employees, developing flexible staffing models, and utilizing telemedicine to expand their reach and capabilities. These efforts have not only helped hospitals meet the immediate needs of the pandemic but have also increased the resilience and adaptability of the healthcare workforce for future emergencies.
Mental Health and Support Systems for Healthcare Workers
Health and well-being of healthcare workers have been significantly impacted by the emotional toll of caring for COVID-19 patients, the fear of exposure to the virus, and the added stress of working in high-pressure environments. Hospitals have recognized the importance of providing mental health support systems, such as counseling services, peer support groups, and resilience training, to help healthcare workers cope with the psychological effects of the pandemic and prevent burnout.
Training and Education During the Crisis
The pandemic has underscored the importance of ongoing training and education for healthcare workers to adapt to rapidly evolving circumstances and ensure the delivery of safe and effective care. Hospitals have ramped up online learning opportunities, simulation exercises, and interprofessional training programs to enhance the skills and knowledge of their staff. Investing in continuous education during the crisis has been necessary in preparing healthcare workers for the challenges of COVID-19 and future public health emergencies.
During the pandemic, hospitals have recognized the critical role of training and education in sustaining a competent and resilient workforce. By prioritizing ongoing learning and skill development, healthcare facilities are better equipped to respond to crises, enhance patient care outcomes, and safeguard the well-being of their staff.
Global Health and International Collaboration
To effectively combat a global health crisis such as the COVID-19 pandemic, international collaboration and unity are paramount. The impact of the virus transcended borders, reiterating the interconnected nature of our world and the need for coordinated efforts among countries to address such challenges with urgency and efficiency.
Cross-Border Medical Aid and Resource Sharing
Resource sharing among countries during the pandemic proved to be a critical lifeline, enabling nations to support each other in times of crisis. Medical personnel, equipment, and expertise were shared across borders to assist regions facing overwhelming challenges. The solidarity demonstrated through this collaborative effort highlighted the importance of a united front in combating a global health threat.
Lessons from International Healthcare Systems
Resource pooling and information exchange from international healthcare systems provided valuable insights during the pandemic response. Countries with robust healthcare infrastructures and well-established pandemic response plans were able to adapt more swiftly to the challenges posed by COVID-19. By studying and learning from these systems, countries can enhance their preparedness for future health crises.
International collaboration revealed stark contrasts in healthcare systems’ capabilities and resilience in the face of a pandemic. While some nations struggled with overwhelmed healthcare facilities and shortages of necessary supplies, others demonstrated remarkable adaptability and efficiency in their response to the crisis.
Future Strategies for Global Pandemic Preparedness
Pandemic preparedness requires a multi-faceted approach that acknowledges the interconnected nature of global health. Establishing early warning systems, improving data sharing mechanisms, and enhancing coordination among countries are necessary components of future pandemic preparedness strategies. By strengthening global health infrastructure and fostering international collaboration, nations can better equip themselves for the challenges posed by infectious disease outbreaks.
Lessons learned from the COVID-19 pandemic underscore the need for proactive and unified efforts in global pandemic preparedness. Investing in healthcare systems, prioritizing research and development of vaccines and treatments, and fostering solidarity among nations are key strategies in mitigating the impact of future health crises.
Preparedness for Future Health Crises
Once again, the world has been reminded of the critical importance of preparedness in the face of health crises. As we reflect on the lessons learned from the COVID-19 pandemic, it is clear that there is much to be done to ensure that our healthcare systems are better equipped to handle future challenges.
Enhancements in Public Health Surveillance
Public health surveillance plays a crucial role in early detection and response to infectious diseases. One key lesson from the COVID-19 pandemic is the need for improved surveillance systems that can quickly detect and track the spread of diseases. Investing in technologies such as real-time data analytics and artificial intelligence can enhance the effectiveness of surveillance efforts, allowing for rapid identification of outbreaks and prompt public health interventions.
Enhancing collaboration between local, national, and international health agencies is also necessary to strengthen public health surveillance. By sharing data and best practices, countries can better coordinate their response efforts and prevent the spread of diseases across borders.
National and International Policy Recommendations
Any future health crisis requires a coordinated and cohesive response at both the national and international levels. Governments and international organizations must work together to develop and implement policies that prioritize public health preparedness and response. This includes establishing clear communication channels, sharing resources, and coordinating efforts to ensure a swift and effective response to outbreaks.
Health organizations must also advocate for increased funding and resources to support public health initiatives and strengthen healthcare systems. Investing in research and development of vaccines, treatments, and diagnostics is necessary to mitigate the impact of future pandemics and ensure the well-being of populations around the globe.
Building Resilience in Healthcare Infrastructure
Crises like the COVID-19 pandemic have exposed vulnerabilities in healthcare infrastructure, highlighting the need for resilience and adaptability. Building robust and flexible healthcare systems that can quickly scale up in times of crisis is necessary to ensuring continuity of care and protecting the health of communities.
Recommendations for strengthening healthcare infrastructure include improving surge capacity, stockpiling necessary medical supplies, and enhancing telehealth capabilities. By investing in infrastructure that can withstand the challenges of future health crises, healthcare organizations can better protect the well-being of patients and healthcare workers.
Conclusion
Taking this into account, the COVID-19 pandemic has significantly impacted hospitals worldwide, revealing vulnerabilities in healthcare systems and highlighting the importance of preparedness. Lessons learned from this crisis emphasize the critical need for hospitals to be adaptable, resilient, and equipped to handle unexpected surges in patient volumes. The rapid response required during the pandemic has underscored the importance of effective communication, collaboration, and coordination between healthcare professionals, government agencies, and the public.
Moving forward, hospitals must prioritize investing in resources, infrastructure, and training to enhance their capacity to respond to future healthcare crises. Strategic planning, regular drills, and contingency preparations are crucial components of ensuring hospitals can effectively manage and mitigate the impact of any future pandemic or emergency. By incorporating the lessons learned from the COVID-19 pandemic, hospitals can better protect their staff, patients, and communities while maintaining the continuity of crucial healthcare services.
Also Refer : The Role Of Hospitals In Mental Health – Promoting Wellness And Recovery
FAQs
Q: What are some key lessons learned by hospitals from the impact of COVID-19?
A: Hospitals have learned the importance of having robust emergency preparedness plans, adequate stockpiles of imperative supplies, the need for effective communication strategies, and the value of collaboration with local and state health departments.
Q: How has the pandemic highlighted the importance of healthcare system resilience?
A: The COVID-19 pandemic has underscored the critical need for healthcare systems to be flexible, adaptable, and able to rapidly scale up or down in response to sudden surges in demand or unexpected challenges.
Q: What measures can hospitals take to improve their preparedness for future public health emergencies?
A: Hospitals can enhance their preparedness by conducting regular drills and exercises, investing in technologies that support telehealth and remote patient monitoring, strengthening supply chain management, and prioritizing the well-being of healthcare workers.
Q: How can hospitals better collaborate with government agencies and other healthcare providers in times of crisis?
A: Hospitals can establish strong partnerships with government agencies, public health departments, community organizations, and neighboring healthcare facilities to share resources, coordinate response efforts, and ensure a unified approach to managing public health emergencies.
Q: What role does data analytics and technology play in helping hospitals respond effectively to healthcare crises?
A: Data analytics and technology solutions enable hospitals to track disease trends, allocate resources efficiently, monitor the impact of interventions, and make informed decisions in real time. Leveraging these tools can enhance hospitals’ ability to respond effectively to healthcare crises and improve patient outcomes.
