There’s no denying the seriousness of hospital acquired infections (HAIs) and the potential risks they pose to patients. These are infections that individuals acquire during their stay at a healthcare facility for treatment of another condition. HAIs can range from relatively mild infections to life-threatening illnesses and can significantly impact a patient’s recovery process.
It is crucial to understand the prevention and safety measures that hospitals implement to minimize the risk of HAIs. By staying informed about these protocols and actively participating in infection prevention practices, patients can play a key role in safeguarding their health while receiving medical care.
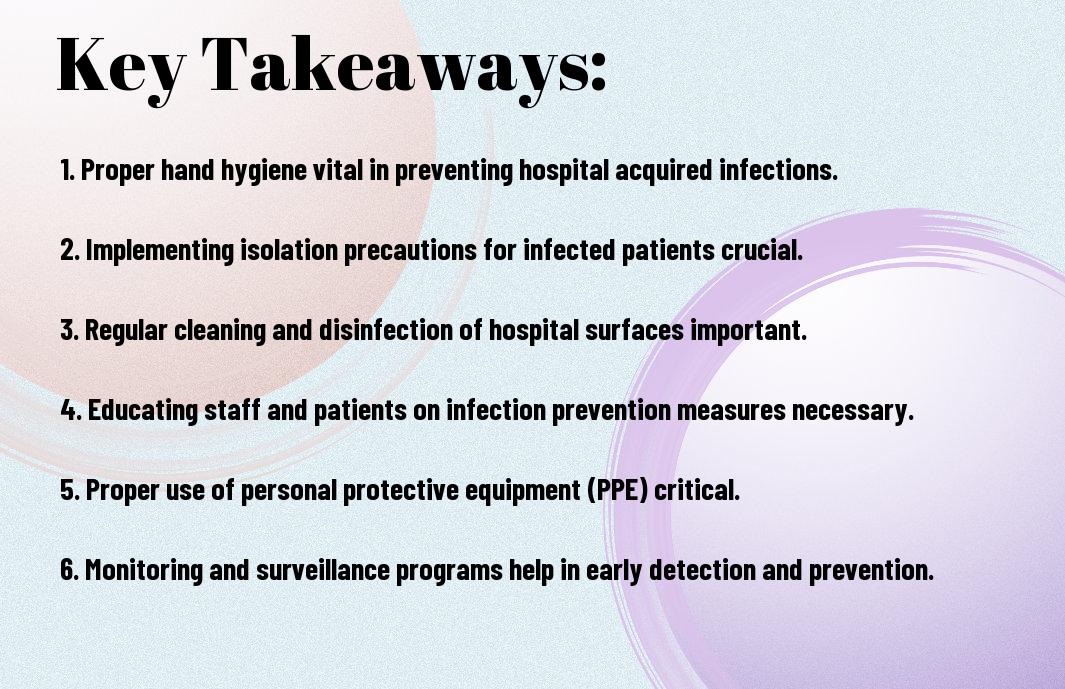
Key Takeaways:
- Preventive Measures: Implement strict hand hygiene protocols, environmental cleaning strategies, and antimicrobial stewardship programs to reduce the risk of hospital-acquired infections.
- Patient Safety: Ensure proper infection control practices are followed at all times, including the use of personal protective equipment and proper disposal of medical waste to protect patients from acquiring infections during their hospital stay.
- Clinical Vigilance: Healthcare providers should remain vigilant for signs of infection in patients, promptly diagnose and treat infections, and closely monitor patients at high risk for hospital-acquired infections to prevent spread and complications.
Also Read : The Importance Of Quality Care In Hospitals – What To Look For In A Healthcare Provider
Defining Hospital Acquired Infections
While hospitals are meant to be places of healing and recovery, they can also pose potential risks to patients in the form of Hospital Acquired Infections (HAIs). These are infections that individuals acquire during their stay in a healthcare facility, which were not present or in the incubation stage at the time of admission.
Types of HAIs
There are various types of HAIs that patients can acquire in a hospital setting. Some common examples include surgical site infections, urinary tract infections, pneumonia, bloodstream infections, and gastrointestinal infections. These infections can be caused by a wide range of pathogens and can lead to prolonged hospital stays, increased healthcare costs, and in severe cases, mortality.
Also Read : Breaking Stereotypes – The Many Specialties And Services Offered In Hospitals Today
| Infections | Types |
| Surgical Site Infections | Infections that occur at the site of a surgery |
| Urinary Tract Infections | Infections affecting the urinary system |
| Pneumonia | Infections primarily affecting the lungs |
| Bloodstream Infections | Infections that enter the bloodstream |
| Gastrointestinal Infections | Infections affecting the digestive system |
Perceiving the risk factors and understanding the types of HAIs is crucial in implementing effective prevention strategies to safeguard patients.
Common Pathogens Responsible for HAIs
Common pathogens responsible for HAIs include bacteria such as Staphylococcus aureus, Escherichia coli, and Pseudomonas aeruginosa. These organisms are adept at surviving in healthcare environments and can pose a serious threat to individuals with weakened immune systems.
For instance, Staphylococcus aureus is a notorious pathogen known for causing surgical site infections and bloodstream infections. Its ability to develop resistance to antibiotics, such as methicillin-resistant Staphylococcus aureus (MRSA), makes it a formidable adversary in healthcare settings.
Also Read : A Guide To Choosing The Right Hospital For Your Healthcare Needs
Understanding the Causes and Risk Factors
Once again, it is necessary to comprehend the causes and risk factors associated with Hospital Acquired Infections (HAIs) to effectively prevent their occurrence.
- Microorganisms such as bacteria, viruses, and fungi play a significant role in causing HAIs.
- Factors like compromised immunity, invasive medical procedures, and prolonged hospital stays increase the risk of acquiring HAIs.
- Patients in intensive care units are more vulnerable to developing infections due to the severity of their illness and the use of invasive devices.
Knowing the underlying reasons and potential risks will enable healthcare providers to implement appropriate preventive measures and safeguard patients from acquiring HAIs.
Also Read : The Future Of Hospitals – How Technology Is Transforming Healthcare
Transmission of Infections in Hospital Settings
One key aspect to consider is how infections are transmitted within hospital settings. In these environments, microorganisms can spread through direct contact, airborne particles, or contaminated surfaces.
Strict adherence to hand hygiene protocols, proper cleaning and disinfection practices, and isolation precautions are vital in controlling the spread of infections within hospitals.
Patient Risk Factors for HAIs
One critical factor in the development of HAIs is the presence of patient-related risk factors. These may include pre-existing health conditions, the use of immunosuppressive medications, or undergoing surgical procedures.
- Patients with weak immune systems, such as those undergoing chemotherapy, are at a higher risk of developing HAIs.
- Individuals with open wounds or surgical incisions are more susceptible to infection.
- Prolonged use of antibiotics can also increase the likelihood of developing antibiotic-resistant infections.
Understanding these patient-related risk factors is crucial in tailoring infection prevention strategies and providing optimal care to prevent the spread of HAIs in healthcare settings.
- Hospital staff must remain vigilant and address any potential risk factors to mitigate the chances of patients acquiring infections.
Patient safety and well-being depend on the proactive identification and management of these risk factors to minimize the incidence of HAIs and ensure quality healthcare outcomes.
Also Read : Building A Career In Hospital Administration – Tips And Insights

Surveillance and Reporting of HAIs
Now, let’s explore into the crucial aspects of surveillance and reporting of Hospital Acquired Infections (HAIs). Monitoring and reporting HAIs are vital for controlling outbreaks, implementing preventive measures, and improving patient safety within healthcare facilities.
Role of Infection Control Programs
The cornerstone of effective surveillance and reporting of HAIs lies in the Infection Control Programs established within healthcare settings. These programs are responsible for monitoring infection rates, implementing preventive strategies, and educating healthcare staff on proper infection control practices. By actively tracking and analyzing data on HAIs, these programs play a vital role in identifying areas of concern and implementing targeted interventions to reduce the risk of infections spreading within the facility.
Control measures put in place by Infection Control Programs not only help in preventing the spread of HAIs but also contribute to overall patient safety and well-being. Regular audits, staff training, and adherence to evidence-based guidelines are key components of these programs, ensuring a comprehensive approach to infection prevention and control.
National and International Reporting Protocols
To facilitate a broader understanding of the prevalence and impact of HAIs, national and international reporting protocols have been established. These protocols require healthcare facilities to report certain types of HAIs to designated authorities, enabling the collation of data at a regional, national, and global level. This data not only helps in identifying trends and emerging threats but also allows for the comparison of infection rates across different healthcare settings and geographical locations.
Prevention Strategies for HAIs
Hand Hygiene
To prevent the spread of Hospital Acquired Infections (HAIs), it is crucial to adhere to proper hand hygiene practices. Keeping hands clean is one of the most effective ways to prevent infections in healthcare settings. To maintain good hand hygiene, healthcare workers should wash their hands with soap and water or use alcohol-based hand sanitizers regularly, especially before and after patient contact.
Remember, hand hygiene is not only important for healthcare providers but also for patients and visitors. Encouraging everyone in the healthcare facility to practice good hand hygiene can significantly reduce the transmission of infectious pathogens and decrease the incidence of HAIs.
Personal Protective Equipment (PPE)
Hygiene measures should also include the appropriate use of Personal Protective Equipment (PPE) in healthcare settings. PPE such as gloves, gowns, masks, and eye protection help to create a barrier between healthcare workers and infectious agents. Proper and consistent use of PPE is vital to protect both patients and healthcare workers from contracting HAIs.
Hand hygiene should always be performed before and after putting on PPE to ensure maximum effectiveness. It is important to follow guidelines on when and how to use PPE correctly to minimize the risk of contamination and infection transmission in healthcare facilities.
Environmental Cleaning and Disinfection
Any surface or equipment that comes into contact with patients should be regularly cleaned and disinfected to prevent the spread of HAIs. Thorough cleaning of high-touch surfaces such as doorknobs, bed rails, and medical equipment is crucial to eliminating harmful pathogens.
Protective barriers and equipment should also be disinfected regularly to maintain a safe and sanitary environment. Healthcare facilities should establish cleaning protocols and ensure that environmental services staff are properly trained to carry out cleaning and disinfection procedures effectively.
Antimicrobial Stewardship
On the front lines of preventing HAIs is the practice of Antimicrobial Stewardship. This involves the responsible use of antimicrobial medications to treat infections, thereby reducing the development of antimicrobial resistance and the spread of multidrug-resistant organisms.
The implementation of antimicrobial stewardship programs in healthcare facilities helps to optimize the use of antibiotics, improve patient outcomes, and minimize the risk of HAIs caused by resistant pathogens. These programs involve a multidisciplinary approach that includes guidelines for appropriate antibiotic prescribing, monitoring of antibiotic use, and education for healthcare providers and patients.
Isolation Precautions
Disinfection measures alone may not always be sufficient to prevent the transmission of certain highly contagious pathogens. In such cases, healthcare facilities may need to implement Isolation Precautions to protect patients and healthcare workers from exposure.
Antimicrobial agents should be used judiciously as part of isolation protocols to prevent the emergence of resistant strains. By isolating patients with specific infections or colonization, healthcare facilities can effectively contain the spread of HAIs and safeguard the health of vulnerable individuals.
The Challenges of Antibiotic Resistance
For Healthcare-associated Infections (HAIs) & Antimicrobial …
The Impact of Antibiotic Resistance on HAIs
Impact: Antibiotic resistance poses a significant threat to healthcare systems worldwide. The overuse and misuse of antibiotics have led to the emergence of multidrug-resistant bacteria, making infections harder to treat. Patients in hospitals are especially vulnerable to these drug-resistant strains, leading to prolonged hospital stays, increased healthcare costs, and higher mortality rates.
Moreover, the spread of antibiotic-resistant infections in healthcare settings contributes to Healthcare-associated Infections (HAIs). These infections not only affect patients but also healthcare workers and visitors, creating a cycle of transmission that can be challenging to break without proper intervention.
Strategies to Combat Antibiotic Resistance
Resistance: To address the growing threat of antibiotic resistance in healthcare settings, it is crucial to implement effective infection control measures. This includes promoting judicious antibiotic use, enhancing surveillance for resistant pathogens, and improving hand hygiene practices among healthcare personnel. Additionally, the development of antimicrobial stewardship programs can help optimize the use of antibiotics and reduce the spread of resistant bacteria.
One key strategy is the promotion of collaboration among healthcare facilities, public health agencies, and policymakers to prioritize infection prevention and control efforts. By working together, stakeholders can share best practices, resources, and data to combat antibiotic resistance and protect patient safety.
Challenges: Despite ongoing efforts to combat antibiotic resistance, the challenges remain complex and multifaceted. The rapid evolution of resistant bacteria, coupled with limited treatment options, emphasizes the urgent need for continued research and innovation in the field of antimicrobial resistance. Addressing these challenges requires a comprehensive approach that involves healthcare providers, policymakers, researchers, and the public working together to safeguard the effectiveness of antibiotics for future generations.
Staff Training and Education
Despite advancements in medical technology and infection control practices, hospital acquired infections (HAIs) remain a significant concern in healthcare settings. One crucial aspect of preventing HAIs is staff training and education. Ensuring that healthcare workers are well-informed, trained, and constantly updating their knowledge is crucial in the fight against HAIs.
Importance of Continuous Learning
Training healthcare staff on the latest infection control protocols, hand hygiene practices, and use of personal protective equipment is crucial in reducing the risk of HAIs. Continuous education helps staff stay updated on changing guidelines, new techniques, and emerging pathogens. It also reinforces the importance of infection prevention practices in their daily routines, promoting a culture of safety within the healthcare facility.
Additionally, ongoing education and training can help healthcare workers recognize potential hazards, improve their response to infectious outbreaks, and enhance their overall infection control practices. By investing in staff training and education, healthcare facilities can significantly reduce the incidence of HAIs and create a safer environment for both patients and staff.
Implementing Effective Training Programs
Importance of establishing structured and comprehensive training programs cannot be overstated. These programs should cover a wide range of topics including infection control principles, best practices for environmental cleaning, proper use of equipment, and patient safety protocols. Implementing regular training sessions, workshops, and simulations can help reinforce key concepts and ensure that healthcare staff are well-prepared to handle infection prevention challenges.
Training programs should also address specific areas of concern within the healthcare facility, tailor-made to the needs of different departments and staff roles. By customizing training programs to address the unique challenges faced by each team, healthcare facilities can effectively improve overall compliance with infection control measures and reduce the risk of HAIs.
Patient and Family Engagement
Many hospital-acquired infections (HAIs) can be prevented through proper patient and family engagement. When patients and their families are actively involved in understanding and implementing infection prevention measures, the risk of acquiring HAIs significantly decreases. Educating patients and families about HAIs and encouraging their participation in prevention efforts are crucial steps to improving patient safety and reducing the prevalence of HAIs in healthcare settings.
Educating Patients and Families about HAIs
Patients and families need to be informed about the potential risks of acquiring infections during a hospital stay. Providing education on common types of HAIs, how they are transmitted, and what preventive measures can be taken is vital. This knowledge empowers patients and their families to actively participate in infection prevention strategies and advocate for their own safety.
Clear communication from healthcare providers regarding infection prevention protocols, such as hand hygiene, isolation precautions, and environmental cleaning, is vital for patients and families to understand their role in reducing the spread of infections. By working together with healthcare staff and following recommended guidelines, patients and families can help create a safer environment for everyone in the healthcare facility.
Encouraging Patient Participation in Prevention
The involvement of patients in their own care is paramount to preventing HAIs. Empowering patients to speak up if they have concerns about their care or notice lapses in infection control practices can help identify potential risks and prevent the spread of infections. Patients should feel comfortable discussing hygiene practices with their healthcare providers and asking questions about the steps being taken to prevent HAIs.
Encouraging patients to be proactive in their own infection prevention can lead to improved outcomes and a reduced risk of HAIs. By actively engaging in hand hygiene, adhering to prescribed guidelines for wound care, and staying informed about their treatment plan, patients play a crucial role in safeguarding their health during a hospital stay.
Educating patients and families about HAIs and involving them in prevention efforts can lead to a more collaborative approach to infection control in healthcare settings. By fostering a culture of shared responsibility and active participation in infection prevention, hospitals can create a safer environment for patients, families, and healthcare providers alike.
Technological Advancements in Preventing HAIs
Innovations in Sterilization and Disinfection
Not only have technological advancements transformed the landscape of healthcare, but they have also played a crucial role in preventing Hospital Acquired Infections (HAIs). Sterilization and disinfection processes have significantly improved with the introduction of advanced technologies. Automated disinfection systems using UV light or hydrogen peroxide vapor have revolutionized the way healthcare facilities clean and sanitize patient rooms, operating theaters, and medical equipment.
On top of that, robotic systems equipped with UV-C lights are being used for thorough disinfection of hospital surfaces, reducing the risk of HAIs caused by surface contamination. These innovations in sterilization and disinfection have dramatically enhanced the safety of patients and healthcare workers alike.
The Role of Health Information Technology
Notably, health information technology has played a pivotal role in preventing HAIs by improving communication, data management, and surveillance in healthcare settings. Electronic health records enable healthcare providers to access patient information efficiently and track infectious diseases more effectively. Real-time monitoring systems can alert healthcare staff to potential outbreaks or deviations from established protocols, allowing for swift intervention to prevent the spread of infections.
One important aspect of health information technology in preventing HAIs is the implementation of computerized physician order entry systems. These systems help reduce medication errors, streamline prescription processes, and ensure that patients receive the right antibiotics at the right time, thus minimizing the risk of antibiotic-resistant HAIs.
Sterilization and disinfection technologies, along with advanced health information systems, are at the forefront of the battle against HAIs. By leveraging these innovations, healthcare facilities can effectively reduce the incidence of infections and create safer environments for both patients and healthcare providers.
Legal and Ethical Considerations
Regulations and Standards Governing HAIs
Unlike community-acquired infections, Hospital-Acquired Infections (HAIs) have specific regulations and standards that govern their prevention and management. These guidelines are put in place to ensure the safety of patients, healthcare workers, and visitors within healthcare facilities. Organizations such as the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) have established protocols to mitigate the risks associated with HAIs.
Adherence to these regulations is crucial for maintaining a safe healthcare environment. Failure to comply with these standards can result in legal consequences for healthcare facilities. By following proper infection control practices and implementing robust prevention strategies, healthcare facilities can reduce the incidence of HAIs and create a safer environment for everyone involved.
Ethical Principles in Infection Prevention and Control
The ethical principles in infection prevention and control play a significant role in the healthcare setting. Healthcare professionals are ethically obligated to provide a safe environment for their patients and to prevent harm whenever possible. This includes taking necessary precautions to prevent the spread of infections, such as following proper hand hygiene protocols and using personal protective equipment.
Considerations: Ethical principles such as beneficence, non-maleficence, and justice guide healthcare providers in making decisions that prioritize patient safety and well-being. By upholding these principles, healthcare professionals can help prevent HAIs and promote a culture of safety within healthcare facilities.
Measuring the Effectiveness of Prevention and Control Strategies
After implementing various prevention and control strategies in hospitals, it is vital to measure their effectiveness to ensure the safety of patients and healthcare workers. By analyzing outcome metrics and performance indicators, healthcare facilities can evaluate the impact of their efforts in reducing hospital-acquired infections (HAIs) and improving overall safety measures.
Outcome Metrics and Performance Indicators
Control measures such as hand hygiene compliance rates, infection rates, and antibiotic stewardship practices are commonly used as outcome metrics to assess the effectiveness of prevention strategies. These metrics provide valuable insights into the success of infection control practices and help identify areas that require improvement. Performance indicators, including surveillance data, compliance audits, and patient outcomes, are crucial in measuring the overall impact of prevention efforts on reducing HAIs.
Outcome metrics also play a vital role in gauging the success of interventions such as environmental cleaning protocols, use of personal protective equipment, and isolation precautions. By regularly monitoring and analyzing these metrics, healthcare facilities can track progress, identify trends, and make informed decisions to further enhance their prevention and control strategies.
Quality Improvement Initiatives
Control measures must be accompanied by quality improvement initiatives to continuously enhance the effectiveness of prevention strategies. These initiatives involve conducting root cause analyses, implementing evidence-based practices, and fostering a culture of safety within healthcare organizations. By engaging healthcare staff in quality improvement projects and providing ongoing education and training, hospitals can continually strive for excellence in infection prevention and control.
Quality Improvement Initiatives focus on measuring the impact of interventions, identifying areas for improvement, and implementing best practices to enhance patient safety. By promoting a proactive approach to infection prevention and control, healthcare facilities can effectively reduce the incidence of HAIs and create a safer environment for all individuals involved in patient care.
Future Directions
For hospitals and healthcare facilities, staying updated on the latest trends and research in hospital-acquired infection (HAI) prevention is crucial for improving patient safety and reducing the burden of HAIs. As we look towards the future, there are promising directions in HAI prevention and infection control policies that can help in further reducing the incidence of HAIs.
Research Frontiers in HAI Prevention
Prevention of HAIs requires a multidisciplinary approach that incorporates cutting-edge research in areas such as antimicrobial stewardship, hand hygiene, environmental cleaning, and innovations in medical devices. Researchers are focusing on developing new technologies and strategies to combat antimicrobial resistance, improve surveillance methods, and enhance infection prevention practices to reduce the risk of HAIs.
Emerging Trends in Infection Control Policies
Trends in infection control policies are shifting towards a more holistic and proactive approach to infection prevention. This includes implementing comprehensive infection control programs, promoting a culture of safety and accountability, enhancing communication among healthcare workers, and leveraging technology for better monitoring and tracking of infections.
As we move forward, healthcare facilities are increasingly adopting evidence-based practices and guidelines, investing in staff education and training, and strengthening their collaboration with public health agencies to stay ahead of emerging infectious threats and improve patient outcomes.
Also Read : The Importance Of Quality Care In Hospitals – What To Look For In A Healthcare Provider
To wrap up
Drawing together the key information about hospital acquired infections, it is evident that prevention and safety measures are crucial in minimizing the risk of such infections. By implementing proper hygiene practices, following infection control protocols, and utilizing antibiotics judiciously, healthcare facilities can greatly reduce the occurrence of HAIs among patients. It is crucial for healthcare providers to work collaboratively to create a safe environment and protect vulnerable patients from preventable infections.
Overall, a comprehensive understanding of the causes, risk factors, and prevention strategies for hospital acquired infections is crucial in promoting patient safety and improving healthcare outcomes. By prioritizing infection prevention measures, healthcare facilities can effectively reduce the burden of HAIs and create a safer environment for both patients and healthcare workers.
FAQ
Q: What are Hospital Acquired Infections (HAIs)?
A: Hospital Acquired Infections (HAIs) are infections that patients acquire during their stay in a healthcare facility that were not present or were incubating at the time of admission.
Q: How do HAIs occur in hospitals?
A: HAIs can occur through various means such as poor hand hygiene practices, inadequate sterilization of medical equipment, contaminated healthcare environments, and transmission from healthcare workers or other patients.
Q: What are the most common types of HAIs?
A: The most common types of HAIs include urinary tract infections, surgical site infections, bloodstream infections, pneumonia, and gastrointestinal infections.
Q: What are the prevention measures for HAIs?
A: Prevention measures for HAIs include proper hand hygiene, sterilization and disinfection of medical equipment, use of personal protective equipment, isolation precautions for infected patients, antimicrobial stewardship, and environmental cleaning.
Q: How can patients protect themselves from HAIs?
A: Patients can protect themselves from HAIs by being proactive in their own care, asking healthcare providers to wash their hands, ensuring that medical equipment is properly sterilized, and following any infection prevention guidelines provided by the healthcare facility.
